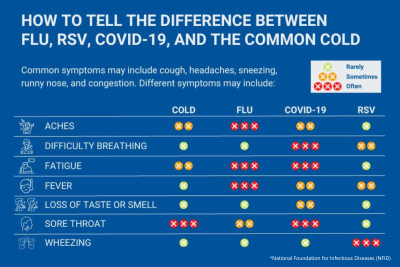
Respiratory viruses are the most frequent cause agents of disease in humans, with significant impact on morbidity (illness/disease) and mortality (death) worldwide, mainly in children (Science Direct). Though hundreds of different viruses can be considered respiratory viruses, we want to provide you with a single place for the latest updates on the following, more prevalent, respiratory illnesses in our community.
FLU
| VACCINES |
|
Flu symptoms can range from mild to severe and include fever, cough, sore throat, fatigue, chills, nausea, runny or stuffy nose, and head and body aches.
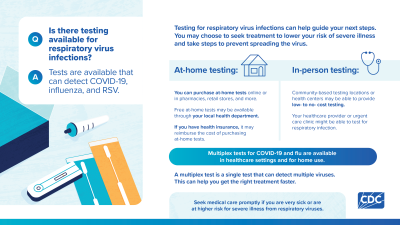
A number of tests are available to detect a flu virus (testing image below). However, while your doctor may test you for flu, not everyone who goes to the doctor with flu-like symptoms will be tested. Although testing is the only way to know if you have flu, your doctor may diagnose you based on your symptoms. Please visit Diagnosing for Flu for more information.
The best way to reduce your risk from seasonal flu and its potentially serious complications is to get vaccinated every year. Vaccines activate the body’s immune response against the flu virus, which can then protect you and your loved ones from severe respiratory illness. It's especially important and effective in the fall and winter when respiratory diseases circulate in higher volumes.
Some people report mild side effects after receiving their flu vaccine, such as headaches, muscle pain, fever, tiredness, and swelling at the injection site. Though side effects might occur, flu vaccines cannot cause flu illness. The risk of side effects is far better than the risk of severe illness without vaccines.
The 2025-26 Flu Vaccine is recommended for everyone ages 6 months and older (AAP, AAFP, CDC, ACOG)*. Protection wanes throughout the season, so October is the best time to get vaccinated.
✓ To get the 2025/2026 flu vaccines, contact a local pharmacy, healthcare provider, or health department. The Cape Girardeau County Public Health Center has the flu vaccine available—contact us for an appointment or check our calendar for the next Drive-Thru Clinic. For specific guidance or questions, talk to your healthcare provider.
For the first time, FluMist, an FDA-approved self-administered nasal spray flu vaccine is available to be delivered to your home! This convenient, at-home option is great for kids who don’t like shots or anyone who doesn’t like needles. Some restrictions apply. Anyone interested in FluMist should talk to their doctor first.
For everyday preventive actions to stop the spread of germs, click here.
Most people with flu have mild illness and do not need medical care or antiviral drugs. If you have flu symptoms, in most cases, you should stay home and avoid contact with other people except to get medical care. For more information about what to do if you get sick, click here.
However, if you're at higher risk of serious flu complications and you get flu symptoms, consult your doctor right away. People at higher risk of flu complications include young children, adults 65 years of age and older, pregnant people, and people with certain medical conditions such as asthma, diabetes and heart disease.
Antiviral drugs are available as treatment but they work best when started early, such as 1-2 days after flu symptoms begin. For people at higher risk of serious flu complications, treatment with influenza antiviral drugs can mean the difference between milder or more serious illness that may result in a hospital stay. For specific guidance or questions, talk to your healthcare provider.
RSV
| VACCINES |
|
People infected with RSV usually show symptoms within 4 to 6 days after getting infected. Keep in mind that almost all children will have had an RSV infection by their second birthday.
Clinical symptoms of RSV are non-specific and can overlap with other viral respiratory or bacterial infections. However, several types of laboratory tests are available for confirming an RSV infection (testing image below). For more information, click here.
The best way to protect those at highest risk for getting severe RSV is by following vaccine recommendations for infants, toddlers, and adults 50 years and older. The RSV vaccine is not currently an annual vaccine. If you received an RSV vaccine already (including last year), you should not get another RSV vaccine at this time (the CDC evaluates how long protection lasts and may update their guidance, as needed). The best time to get vaccinated is in late summer and early fall.
Side effects such as pain, redness, and swelling where the shot is given, fatigue, fever, headache, nausea, diarrhea, and muscle or joint pain may occur. If they do, they're usually mild. The benefits of RSV vaccination far outweigh the potential risk of severe disease.
The RSV Vaccine is recommended for all infants <8 months, children 8-19 months with risk factors, all pregnant individuals during weeks 32-36 of their pregnancy, all adults 75+ years old, and adults 50-74 years old with risk factors (AAP, AAFP, CDC, ACOG)*. For an easy guide, click here.
✓ To get the RSV vaccine, contact a local pharmacy, healthcare provider, or health department. The Cape Girardeau County Public Health Center has the RSV vaccine available for adults—contact us for an appointment or check our calendar for the next Drive-Thru Clinic. For vaccinating infants or children, please consult your pediatrician. For specific guidance or questions, talk to your healthcare provider.
For everyday preventive actions to stop the spread of germs, click here.
Most people who get an RSV infection will have mild illness and will recover in a week or two. There is no treatment, but you can manage symptoms with over-the-counter medications. For steps to relieve symptoms, click here.
However, if there is difficulty breathing, not drinking enough fluids, or worsening symptoms, contact your doctor right away. Infants, young children, and older adults are more likely to develop severe RSV infection and may need to be hospitalized.
COVID-19
| VACCINES |
|
COVID-19 symptoms can include fever, chills, cough, sore throat, shortness of breath, runny or stuffy nose, head or body aches, and new loss of taste or smell. People who are infected have a wide range of symptoms, from mild to severe, that may appear 2-14 days after exposure to the virus. For some, symptoms start as mild but will progress to more severe.
- If you have symptoms: test immediately.
- If you don't have symptoms but have been exposed: wait at least 5 full days after your exposure before testing (testing too early may yield inaccurate result)
COVID-19 testing can help you know if you have COVID-19 so you can decide what to do next, like getting treatment to reduce your risk of severe illness and taking steps to lower your chances of spreading the virus to others (testing image below). There are two kinds of tests available to diagnose COVID-19: tests for current infection (viral tests) and tests for past infection (antibody tests). Please visit Testing for COVID-19 for more information.
Medical societies and research continue to reaffirm that the COVID-19 vaccine remains one of the safest and most effective ways to protect all children, adults, and pregnant people against severe illness and hospitalization. Like the flu, new variants of covid emerge and is why updated vaccines are necessary. The best time to get vaccinated is now; if you were recently infected, you can wait 4-6 months.
Side effects such as soreness at the injection site, achiness or joint pain, fatigue, slight fever, chills, or nausea are normal and not cause for concern. They're a sign that your body is learning an immune response—as it’s supposed to do. If you get side effects, they generally subside within 1-2 days. Vaccine-induced immunity is far better than getting infected because the risk of complications from natural infection with COVID greatly outweighs any slight risk of side effects from COVID-19 vaccines.
The 2025/2026 COVID-19 Vaccine is recommended for children 6-23 months old, children 2-18 years old (with risk factors or if parent wants it), and all adults (AAP, AAFP, ACOG, CDC)*. We understand there may have been confusion while the CDC completed its process of reviews, but there is now clear guidance: the vaccine is recommended by the federal government and professional medial organizations for everyone 6 months and older.
Everyone ages 6 months and older, regardless of their high risk for severe COVID-19, should talk to their healthcare provider about what's best for them based on age, vaccination history, and other factors. We provide evidence-based information and are required to follow CDC's vaccine recommendations; we also are committed to ongoing vaccine access and affordability.
✓ To get the 2025/2026 COVID-19 vaccine, contact a local pharmacy, healthcare provider, or health department. The Cape Girardeau County Public Health Center has the covid vaccine available—contact us for an appointment or check our calendar for the next Drive-Thru Clinic. For specific guidance or questions, talk to your healthcare provider.
✓ The 2025/2026 COVID-19 vaccine does not require a prescription order in most states. This availability map is a helpful reference or you may contact your local pharmacy, healthcare provider, or our health center to ask.
For additional prevention strategies, click here.
Most people with COVID-19 have mild illness and can recover at home. You can treat symptoms with over-the-counter medicines. Just be sure to stay home and avoid contact with other people to protect others, especially loved ones who may be vulnerable to more severe illness. For more information about what to do if you get sick, click here.
However, if you have risk factors for severe illness contact your doctor for testing and/or treatment right away. If you feel trouble breathing, persistent pain or pressure in the chest, new confusion, inability to wake or stay awake, or lips, nail beds and skin that appear pale, gray, or blue, seek emergency help.
There are several antiviral medications used to treat mild to moderate COVID-19 in people who are more likely to get very sick. They can help lower your risk of severe illness. Don't delay: they must be started within 5-7 days after you first develop symptoms to be effective. To learn more about the types of COVID-19 treatments, click here.
*Medical societies: American Academy of Pediatrics (AAP), American College of Obstetricians and Gynecologists (ACOG), American Academy of Family Physicians (AAFP)
Sources: Centers for Disease Control and Prevention (CDC), Your Local Epidemiologist (YLE), Common Health Coalition, Public Health Communications Collaborative (PHCC), John Hopkins Bloomberg School of Public Health
Updated: 10/20/25